Healthy beginnings: applying All Our Health
Updated 18 July 2024
Note: the Public Health England team leading this policy transitioned into the Office for Health Improvement and Disparities (OHID) on 1 October 2021.
Introduction
This guide is part of ‘All Our Health’, a resource which helps health professionals prevent ill health and promote wellbeing as part of their everyday practice. The information below will help health care professionals and care staff use their trusted relationships with children, families and communities to promote the benefits of promoting the best start in life.
We also outline important actions that managers and staff holding strategic roles can take. View the full range of ‘All Our Health’ topics.
Access the healthy beginnings e-learning session
An interactive e-learning version of this topic is now available to use.
The Office for Health Inequalities and Disparities (OHID) and Health Education England’s ‘e-Learning for Healthcare’ have developed this content to increase the confidence and skills of health and care professionals, to embed prevention in their day-to-day practice.
Promoting Best Start in Life in your professional practice
Many health challenges and inequalities have foundations in early childhood, with the poorest families experiencing the worst health outcomes. Reducing child health inequalities, what’s the problem? reports that adverse health outcomes would be reduced by 18% to 59% if all children were as healthy as the most socially advantaged.
The Royal College of Paediatrics and Child Health (RCPCH) report, State of child health - England: 1 year on, highlights that children living in England have poorer health outcomes than average across the EU15+ (the 15 EU countries plus Canada, Australia and Norway), including infant mortality, child obesity and low rates of breastfeeding.
The Health profile for England, which indicates that overall child health in England has continued to improve.
However, children who live in more deprived areas were more likely to:
- be exposed to avoidable risks before birth
- get off to a less healthy start from birth
- experience poor outcomes by the time they start school - when compared with children who live in less deprived areas
Health inequalities are seen across all indicators presented. Health inequalities are not inevitable and can be significantly reduced; however, focusing solely on the most disadvantaged will not reduce health inequalities sufficiently. To reduce the steepness of the social gradient in health, actions must be universal, but with a scale and intensity that is proportionate to the level of disadvantage. Marmot (2010) (PDF, 16.2MB)
All Our Health takes an ecological approach to improve outcomes for children by addressing the child as an individual within the context of his or her family, community and the wider system in which children and families live.

The first 1001 days (from conception to age 2) are recognised as a crucial period during which the foundations for future health and wellbeing are built. Positive experiences - and good quality parent-infant relationships during this time - are associated with the formation of a secure attachment which contributes to good physical and mental health, speech and language development, emotional self-regulation, resilience and wider social and economic advantages throughout the life course.
A healthy pregnancy and early years are important to the health of the developing baby. There is a growing body of evidence and research on neurological development, epigenetics and the impact of stress, anxiety and adverse experiences in pregnancy and the first years of life. This reiterates the importance of prevention, support for parents and early intervention.
Pregnancy and the early years provide an ideal opportunity for public health practitioners and other professional groups to advise and support parents on a range of issues including:
- pre-conception care - to improve planning and preparation for pregnancy
- quitting smoking, to increase the number of women having a smoke-free pregnancy
- alcohol avoidance in pregnancy to reduce risk of long-term harm to the baby
- healthy eating habits, to increase the number of women entering pregnancy with a healthy weight and to increase the number of babies breastfed at 6 months
- health protection to maximise the benefit from the full maternal and child immunisation; and antenatal and newborn screening programmes provided by the NHS
- transition to parenthood, to support parents to make a positive emotional transition to parenthood and to reduce the burden of perinatal mental illness by improving access targeted and specialist interventions if needed
Preconception support
Health before and during pregnancy is vital. A healthy woman is more likely to give birth to a healthy baby. Health professionals should support women (and their partners) to adopt positive health behaviours and reduce risk factors. Pre-conceptual care includes ensuring full immunisation status, advice on vitamins, and folic acid and advice on alcohol and tobacco and on nutrition.
A number of resources have been developed to help in planning and preparation for pregnancy, to improve outcomes for mothers and babies including making the case for preconception care, a report for local maternity systems and their wider systems partners.
The report is accompanied by these additional resources:
- infographic summary document
- toolkit for health of women before and during pregnancy
- national report on risk factors and inequalities.
- preconception animation
Between pregnancies, advice on family spacing, contraception services is important. Researchers of The prevalence of unplanned pregnancy and associated factors in Britain: findings from the third national survey of sexual attitudes and lifestyle identified that 45% of pregnancies in the UK are unplanned or associated with feelings of ambivalence. Pregnancies in young, single women are most likely to be unplanned.
Pregnancy
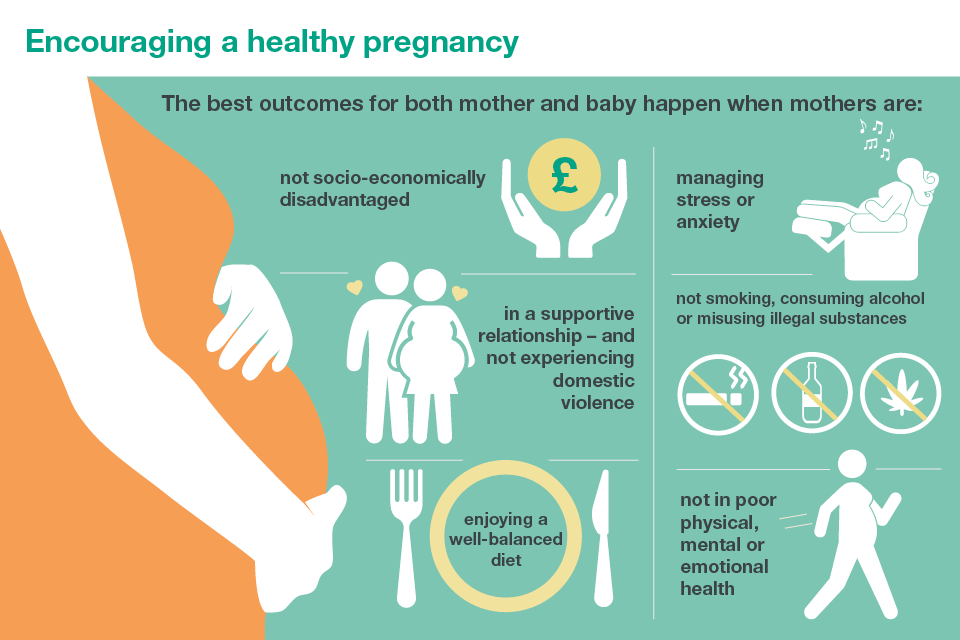
There are a number of factors that can increase the risk of harm to the unborn baby and many of these are influenced by health inequalities.
The Health Secretary announced his ambition to reduce stillbirth, neonatal death and maternal death by 50% by 2030. In January 2019, that ambition was accelerated to achieve 50% reductions in stillbirth, maternal mortality, neonatal mortality and serious brain injury by 2025.
In January 2016, Better births: a 5 year forward view for maternity care was published, with recommendations for all sectors of health and social care to make to improve maternity outcomes.
Achieving this requires a coordinated response, which includes prevention focus on risk factors such as smoking, alcohol, weight and mental health, during maternity and pre-conception.
Early weeks and months of life
Breastfeeding
Breastfeeding is an important public health priority. Supporting families to breastfeed and increasing the number of babies who are breastfed gives babies the best possible start.
Breastfeeding improves infant and maternal health and wellbeing in both the short and longer term and research demonstrate:
- exclusive breastfeeding should be recommended for around the first 6 months of life - with continued breastfeeding alongside solid foods for at least the first year of life
- improving breastfeeding rates in lower socioeconomic groups and young parents can play an important role in reducing health inequalities
- responsive feeding has benefits for mother and infant, including emotional attachment
- protection against the risk of respiratory infections, gastroenteritis and ear infections in breastfed infants
- improved oral health and reducing tooth decay in breastfed infants
- reduced risk of Sudden Unexpected Deaths in Infancy in breastfed babies
Breastfeeding can be protective against obesity, particularly in those who are genetically predisposed; breastfeeding for 3 months in the first year of a baby’s life reduces the risk of obesity by 13% in later life. Additionally, mothers who breastfeed benefit from a faster return to pre-pregnancy weight.
Early years high impact area 3 supports breastfeeding initiation and maintenance with links to evidence and resources.
Emotional health and wellbeing
The earliest experiences, starting in the womb, shape a baby’s brain development. During the first 2 years of life, the brain displays a remarkable capacity to absorb information and adapt to its surroundings.
Positive early experiences can improve the child’s readiness to learn, school-readiness and longer-term life chances. Positive influences include:
- responsive parenting, and the quality of parent-child interaction
- socio-economic status and access to resources like books, toys and home learning experiences
- access to high-quality early education and care
Parents are critical in children’s social and emotional wellbeing. The parent-child relationship is particularly important. Positive emotional development during infancy and early childhood is associated with early language and communication development, school readiness and positive emotional adjustment in later life.
Early years high impact area 1 supports the transition to parenthood with links to the evidence and resources.
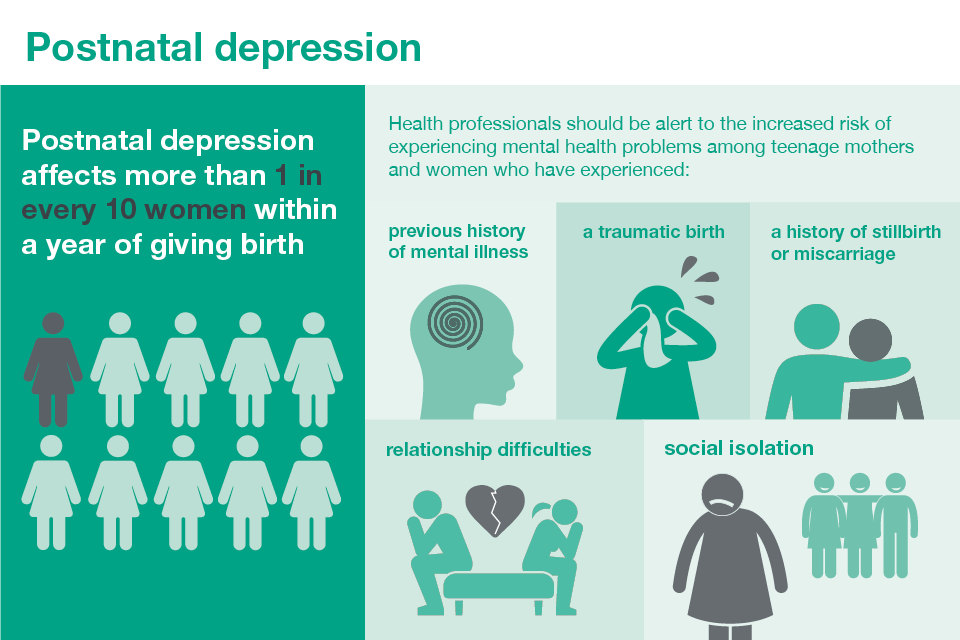
Mental health issues can impact on a mother’s ability to bond with her baby and be sensitive and attuned to the baby’s emotions, early communication and needs. This can affect the baby’s ability to develop a secure attachment and early language development.
Early years high impact area 2 supports interventions for good maternal mental health with links to evidence and resources.
Early speech, language and communication skills
The first years of life provide an important opportunity to ensure every child has the support and environment to reach their full potential. The ability to communicate is a fundamental life skill, which directly impacts on the child’s ability to learn, develop friendships and future life chances.
There is increasing concern about the numbers of children starting school with poor speech, language and communication skills with unacceptable differences in outcomes in different areas of the country. Disparities in early language development are recognisable in the second year of life and have an impact by the time children enter school. Around two-fifths of disadvantaged 5-year-olds do not meet the expected literacy standard for their age.
Language development is determined by genetic inheritance and is also very sensitive to socio-economic deprivation and the quality of input children receive from the adults around them. More than 10% of children and young people have long-term speech, language and communication needs (SLCN). This can be a barrier to communication or learning, with children from socially disadvantaged families more than twice as likely to be diagnosed with a language problem. Due to social clustering, more than 50% of children living in areas of high social deprivation may start school with SLCN.
Early language is recognised as a primary indicator of child wellbeing due to the link between language and other social, emotional and learning outcomes.
Without support, children and young people with speech, language and communication need risk underachievement, mental health problems and poor life chances.
Educational attainment
15% of pupils with identified SLCN achieved the expected standard in reading, writing and mathematics at the end of their primary school years compared with 61% of all pupils.
Only 20.3% of pupils with SLCN gained grade 4/C or above in English and Maths at GCSE, compared with 63.9% of all pupils.
Social, emotional and mental health
81% of children with emotional and behavioural disorders have unidentified language needs.
Children with vocabulary difficulties at age 5 are 3 times more likely to have mental health problems in adulthood and twice as likely to be unemployed when they reach adulthood.
Lifelong impact
88% of long-term unemployed young men have been found to have SLCN.
60% of young offenders have low language skills.
Babies are born ready to communicate; midwifery, health visiting and Early Years services are well placed to promote parental attunement during pregnancy and the first few years of life to support parents to recognise and respond to their baby’s individual cues and gestures which provide the foundation for future language.
The preschool years present a prime opportunity to promote the language and communication of all children and identify those children who are not developing as expected and may require targeted and specialist intervention.
Being ‘healthy and ready to learn’ at age 2 and ‘ready for school at age 5’ gives every child the best start in life. From about 18 months the gap between those children who are developing as expected and those who are not begins to widen.
The mandated health reviews provide an ideal opportunity to promote language development and identify those children who would benefit from additional support or targeted early intervention. Many of the signs of developmental delay and poor health outcomes can be recognised at this age. Help should be offered early so that children do not start school already behind their peers.
Early years high impact area 6 provides links to evidence and resources for the health, wellbeing and development of the child aged 2.
The Early Intervention Foundation work with government departments and leading academics to evaluate early interventions and support the embedding of this evidence in practice. Full details on evaluated programmes can be found in The Foundations for Life Report, The Rapid Review of the Healthy Child Programme and the EIF Guidebook with evidence-based early interventions which improve outcomes for children and reduce long term health and social costs later in the course of life.
Healthy weight and physical activity
Obesity is strongly related to socioeconomic status and deprivation in children. Among children in reception (aged 4 to 5) almost a quarter are overweight or obese and children from the most deprived areas are twice as likely to be obese than those from the least deprived areas. The early years offer an opportunity to promote healthy eating and physical activity that could be maintained through life.
Early years high impact area 4 supports healthy weight and good nutrition with links to evidence and resources For infants who are not yet walking, physical activity refers to movement of any intensity and may include:
- ‘tummy time’ – this includes any time spent on the stomach including rolling and playing on the floor
- reaching for and grasping objects, pulling, pushing and playing with other people
- ‘parent and baby’ swim sessions
Minimising sedentary behaviour is also important for health and development and may include:
- reducing time spent in infant carriers or seats
- reducing time spent in walking aids or baby bouncers (these limit free movement)
- reducing time spent in front of TV or other screens
Once walking, pre-schoolers should be physically active for at least 3 hours, spread throughout the day, to develop movement and coordination, improve cardiovascular and bone health and contribute to a healthy weight (CMO Physical Activity for Early Years).
The promoting healthy weight in children, young people and families resource has been developed to support local authorities, NHS commissioners and providers, voluntary and community sector organisations to take action to reduce obesity.
Reducing unintentional injuries
Reducing unintentional injuries in childhood remains an important public health priority. Unintentional injuries in and around the home are a leading cause of preventable death for children under 5 years and are a major cause of ill health and serious disability. The majority of unintentional injuries are preventable and they disproportionately affect children living in socioeconomic disadvantage.
Even when local authorities have child injury rates that are similar to those for England, this may mask significant inequalities between smaller geographical areas (districts, wards) within local authorities which need addressing. Local authorities should consider not only the overall child injury rate but also the extent of inequalities in child injury rates across smaller geographical areas when deciding what child injury prevention actions are required.
Data analysis shows that the emergency hospital admission rate for unintentional injuries among the under 5s is 42% higher for children from the most deprived areas compared with children from the least deprived, and for some injury types this inequality may be much larger. These inequalities support the targeting of preventative interventions to children and young people living in the most deprived areas.
Early years high impact area 5 promotes health literacy, accident prevention and the management of minor illnesses with links to evidence and resources.
A number of resources have been published to support local authorities and practitioners working with families including:
- preventing unintentional injuries: a guide for all staff working with children under 5 years
- local data to support these on the Fingertips site
Reducing unintentional injuries in and around the home among children under 5 years sets out 3 action areas that aim to reduce the numbers of children injured and killed and describes 4 steps local partnerships can take to build robust injury prevention strategies.
Core principles for health and care professionals
Healthcare professionals should:
- understand the needs of families, communities and population and the services available for children and young people
- think about the resources to support the best start in life available in the health and wellbeing system
- understand specific activities which can prevent, protect, and promote the best start in life
Taking action
Population level
Front line health or care professionals
Health and care professionals can have an impact through taking various actions, which are detailed below. These are particularly applicable to midwives and health visitors.
Useful actions include:
- leading the delivery of the Healthy Child Programme, and the ‘health visitors 4-5-6 model’
- providing interventions in the six early years high impact areas which focus on the areas having the biggest impact on a child’s life
- working in partnership with parents to develop a shared understanding of the things that matter most to the family; using active listening skills and a non-judgmental, asset-based approach when working with parents and encouraging parents to talk about their feelings
- developing their own goals and plans to improve their health and wellbeing
- completing the HCP e-learning for health module on child development and attending training sessions to ensure skills and knowledge are up to date
- providing consistent evidence-based healthier weight, optimal nutrition and physical activity messages during preconception and maternity, and from birth to 5 years
- supporting parents in their decision-making, and ensuring they have evidence-based information
- providing public health protective and preventive advice and interventions, as part of antenatal care pathway
- supporting smoke-free pregnancy: national guidance from the National Institute for Health and Care Excellence (NICE) outlines interventions to support stop smoking in pregnancy and following childbirth
- giving advice on nutrition and physical activity; energy needs do not change in the first 6 months of pregnancy and increase only slightly in the last 3 months, by around 200 calories per day
- giving encouragement to be physically active during pregnancy
- giving advice on folic acid and vitamin supplements
- giving advice that when planning a pregnancy and whilst pregnant the safest approach is not to drink alcohol UK Chief Medical Officers’ alcohol guidelines review
- acting as a champion for the benefits of breastfeeding, and providing early support to help women address any problems
- supporting the transition to parenthood and first 2 years
- supporting early identification of perinatal mental health problems - providing evidence-based interventions and signposting, to specialist support where needed using NICE guidance on postnatal depression
- promoting the Start4Life campaign, providing parents and parents-to-be with trusted NHS advice on pregnancy and early years
Additional actions that can be taken, include:
- promoting and providing newborn screening programmes and childhood immunisations programme
- working with parents and early years settings to provide an integrated review at age 2 for all children using ‘ASQ-3 BE’ and ‘ASQ-SE’, as part of a holistic assessment of health, growth and development; to identify children who are not developing as expected, and to work with families to promote development and targeted interventions as indicated
- encouraging parents to register their child with the dentist, and receive their first dental health check by one year using OHID’s oral health toolkit
- providing early help and access to local services for children and families who may need additional support, at times when they need it most
- recognising signs of maltreatment, and responding to safeguarding concerns in accordance with Working together to safeguard children, 2018 to receive sufficient training and supervision to ensure that they are up to date with local policies and procedures for working in safeguarding or child protection
- improving service access through technology and safe social media approaches which complement face-to-face delivery
- using supervision as a supportive tool, to address emotive issues from practice and promote resilience
Team leaders or managers
Team leaders or managers can take practical actions to promote the best start in life. For instance:
- leading and providing the Healthy Child Programme, and building community assists as part of the ‘health visitors 4-5-6 model’
- developing integrated services between health, education providers, the community and third sector organisations, to ensure they are responsive to national and local needs and demonstrate improved public health outcomes
- being aware of local services and place-based activities, making communities healthy places for children and families
- creating and raising awareness of the importance of community parenting programmes, that offer social support to parents in the early years
- advising on access to programmes such as Healthy Start
- using available technology to improve access to support and information for parents - for example, the baby buddy app
- being aware of NICE guidance, health and social care commissioners, specialists in domestic violence and others who may bring them into contact with people who experience or perpetrate domestic violence and abuse
Senior or strategic leaders
Strategic managers should be aware of interventions and practical actions they can take, which include:
- promoting the understanding of the important of the pregnancy and first 2 years of life, for children’s future health and wellbeing
- supporting Building Great Britons, and raising awareness of this crucial time in early brain development
- supporting the Unicef UK Baby Friendly Initiative, which aims to improve breastfeeding rates and the attachment and nutrition of all infants
- using OHID’s needs assessment tool to help local commissioners and providers, to plan their approach to perinatal and infant mental health in their area; the new tool provides evidence-based information on risk factors affecting perinatal and infant health
Examples of good practice
Understanding local needs
The following sources of data can help health and care professionals understand their local needs.
To gain an overview of the sources of data available from Public Health England, which can help health and care professionals understand their local needs, begin by visiting Child and maternal health data and intelligence: guide for health professionals.
Health and care professionals who are particularly interested in the early years may find the following of interest:
-
Collections of indicators for the early years and breastfeeding available through the Fingertips tool. This includes information about low birthweight, smoking in pregnancy, breastfeeding, immunisations, teenage pregnancy and infant mortality as well as child development outcomes at 2 to 2 ½ years using the Ages and Stages questionnaire-3 (ASQ-3) (PDF, 349KB). Many of the indicators are also included in the Public Health Outcomes Framework.
-
NHS Digital also publishes data from the Maternity Services Data Set and the Community Services Data Set. These include information about a variety of indicators related to child and maternal health.
Measuring impact
As a health and care professional, there are a range of reasons why it makes sense to measure your impact and demonstrate the value of your contribution. This could be about sharing what has worked well in order to benefit your colleagues and local people, to support commissioning decisions or help you with your professional development.
The Everyday interactions measuring impact toolkit provides a quick, straightforward and easy way for health and care professionals to record and measure their public health impact in a consistent and comparable way.
The healthy beginnings impact pathway is recommended for healthcare professionals to record and measure actions undertaken as part of routine care which impact on adult obesity.
Further reading, resources and good practice
Examples of good practice
The Healthy Child Programme
The Healthy Child Programme, the healthy child programme (0 to 5 years) rapid review and Best Start in Life and Beyond (PDF, 1.4MB) documents describe the transformed 4-5-6 health visiting universal preventative model which focuses on giving every child the best start in life.
The documents provide a framework to support collaborative working and integrated services to improve health outcomes in response to local need. The programme provides families with screening, immunisation, health and development reviews, prevention, and early intervention.
Health visitors lead the delivery of the programme in collaboration with other health and early years professionals to support families to give their children the best start in life. This is delivered as a universal service with additional services for families needing extra support, whether short-term intervention or ongoing help for complex longer-term problems.
Mandated universal health and development reviews are an important feature of the Healthy Child Programme, and take place at:
- 28 weeks of pregnancy
- within 14 days of birth
- 6 to 8 weeks
- 9 to 12 months
- 2 to 2.5 years
The universal service facilitates the early identification of children and families who are at risk of poor outcomes and in need of additional support, through effective assessment of need using an ecological approach. Using an asset-based approach and the health-promoting principles of Making every contact count (MECC), and NICE public health guidance, health visitors promote healthy lifestyles and the value of ‘health’ as a foundation for future wellbeing at all universal contacts.
Health visitors build parental confidence in making positive changes to protective factors like healthy eating, physical activity, accident prevention, dental health, and responsive parenting. The programme can ensure families receive early help and support upstream before problems develop further and reduce demand on downstream, higher cost specialist services.
Healthy Start
Healthy Start is a UK-wide government scheme, embedded within the Healthy Child Programme, to improve the health of low-income pregnant women and families on benefits and tax credits.
Healthy Start provides a great opportunity for health professionals and others working with pregnant women and families to offer encouragement, information and advice on issues such as healthy eating, breastfeeding and vitamins. Vouchers can be used to help families on a low-income buy some basic foods, such as milk and fresh or frozen fruit.
The Early Intervention Foundation Guidebook is an online resource of evidence-based interventions of ‘what works’ in the early years.
The UK Baby Friendly Initiative is based on a global accreditation programme of Unicef and the World Health Organisation and includes baby friendly standards. It is designed to support breastfeeding and parent-infant relationships, by working with public services to improve standards of care.
The MBRRACE Report ‘Saving Lives, Improving Mothers’ Care’ includes data on surveillance of maternal deaths between 2012 and 2014. It also includes Confidential Enquiries for women who died between 2009 and 2014 focusing on lessons about cardiovascular disease, caring for women with hypertensive disorders of pregnancy, and messages for early pregnancy and critical care.
The Marmot Review Fair Society Healthy Lives proposed the most effective evidence-based strategies for reducing health inequalities in England from 2010. It includes 2 specific policy areas for children:
- Give every child the best start in life.
- Enable all children, young people and adults to maximise their capabilities and have control over their lives.
The six early years high impact areas: priority areas identified by the Local Government Association and Department of Health are:
- transition to parenthood
- maternal mental health
- breastfeeding
- healthy weight and healthy nutrition
- management of minor illness and reducing accidents
- health, well-being, and development of the child aged 2
A 0 to 19 commissioning guidance has been developed, which is a range of data analysis tools to help local commissioners and providers plan their services and identify local priorities.
Local authorities, health visiting services and early years providers are expected to work together to ensure that children receive an integrated review at 2 to 2.5 years. The National Children’s Bureau (NCB) has produced materials to support this approach.
The Family Nurse Partnership programme provides a targeted service for first-time mums aged up to 24, in line with local area eligibility criteria, until their child is up to 2 years old.
Early intervention: the next steps is a report about interventions in children’s earliest years that can eliminate or reduce costly and damaging social problems.
Educational outreach interventions aimed at reducing antibiotic use in children include:
- Reducing antibiotic use in children: a randomised trial in 12 practices on enrolled children under 6
- An evidence-based approach to reducing antibiotic use in children with acute otitis media: controlled before and after study
Professional resources and tools
NICE guidance
Behaviour change: general approaches (PH6) is aimed at those responsible for helping people to change their behaviour to improve their health.
Behaviour change: individual approaches (PH49) also makes recommendations on individual-level interventions aimed at health-damaging behaviour in over 16s.
Pregnancy and complex social factors: a model for service provision for pregnant women with complex social factors (CG110) describes how access to care can be improved for pregnant women with complex social factors.
Weight management and nutrition
Maternal and child nutrition (PH11) relates to pregnant women (and those who are planning to become pregnant), mothers and other carers of children aged under 5 and their children. It is particularly aimed at those on a low income or from a disadvantaged group.
In addition, Weight management before, during and after pregnancy: guidance (PH27) provides evidence-based recommendations to help all pregnant women eat healthily and keep physically active.
Vitamin D: increasing supplement use among at-risk groups (PH56) aims to increase supplement use to prevent vitamin D deficiency among at-risk groups.
Promoting physical activity for children and young people (PH17) also provides guidance for all those who are involved in promoting physical activity among children and young people, including parents and carers.
Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children (CG43) is the first national guidance on the prevention of overweight and obesity in adults and children in England and Wales.
Social and emotional wellbeing
Social and emotional wellbeing: early years (PH40) aims to define how the social and emotional wellbeing of vulnerable children under 5 years can be supported.
Antenatal and postnatal mental health (CG192) offers evidence-based advice on the care and treatment of mental health problems during pregnancy and postnatal, and in women planning pregnancy.
NICE has produced guidance on antenatal and postnatal mental health (CG192) which can help health professionals recognise the signs of mental health problems and to select the appropriate treatment.
Smoking
Stop smoking interventions and services (NG92) provides guidance on smoking cessation for health and care professionals working in local health services.
Smoking: stopping in pregnancy and after childbirth (PH26) includes recommendations for those planning a pregnancy or who have an infant under 12 months.
Preventing unintentional injuries
Unintentional injuries: prevention strategies for under 15s (PH29) gives advice and guidance on preventing unintentional injuries in the home, on the road and during outdoor play and leisure.
Unintentional injuries on the road: interventions for under 15s (PH31) gives advice on how healthcare professionals and local highways authorities can make the roads safer.
Unintentional injuries in the home: interventions for under 15s (PH30) aims to prevent unintentional injuries among all children and young people but in particular, those living in disadvantaged circumstances, as they are at increased risk compared to the general population.
Postnatal
Postnatal care (CG37) offers evidence-based advice on the care of women and babies in the 6 to 8 weeks after birth.
Atopic eczema in under 12s: diagnosis and management (CG57) covers the management of atopic eczema in children from birth up to the age of 12 years.
Division of ankyloglossia (tongue-tie) for breastfeeding (IPG149) is guidance and resources on the procedure of the division of tongue-tie.
There is a range of additional NICE guidance documents which are relevant to Early years high impact area 6 - Health, Wellbeing and Development of the Child Age 2.
Child maltreatment: when to suspect maltreatment in under 18s (CG89) covers the alerting features in children and young people.
Immunisations: reducing differences in uptake in under 19s (PH21) aims to increase immunisations uptake among under 19s from groups where uptake is low.
Approaches for oral health improvement for local authorities and their partners (PH55) makes recommendations on undertaking oral health assessments, local strategies and community-based interventions.
